Psychiatric disorder is more common than we may think. One such common disorder, which could be linked to our increasingly busy, isolated and stressful lives, is bipolar disorder. What is bipolar disorder, what happens in the brain, and how do friends and loved ones help a person who may suffer with it?
By Dr Samantha J. Brooks Ph.D.
 Bipolar disorder – a mood disorder characterised by polar
extremes of mood – was once known as “manic-depressive disorder”, which sheds light on the symptoms of this often debilating psychiatric condition.While it is normal to experience fluctuating periods of happiness and sadness associated with usual life circumstances, a
person diagnosed with bipolar disorder will have triggered swings from extreme
happiness and high levels of energy, to extreme sadness and hopelessness,
within a matter of hours or days. Extreme happiness presents as mania, such
that a person becomes excessively active in behaviour and speech, finds it
difficult to sleep or sit still without fidgeting, and may have racing thoughts
and ideas that fly quickly through the mind in illogical succession. A person in the manic phase may take more
risks, such as being more sexually active, taking drugs or spending more
money. Compare the manic phase to
extreme sadness, where a person may experience debilitating depression and
limited energy. During the depressive
phase a person may sleep all day and feel as if everything in their world is
hopeless, with no motivation to change things. Both extremes are like a see-saw
for the individual with bipolar disorder, who will likely experience no sense
of organisation or control over their life. The extremes of bipolar disorder
are associated with fluctuating neurotransmitter levels in the brain – a
significant rise in dopamine levels for mania and a significant drop in
serotonin and opioid levels for depression.
Less extreme versions of this debilitating condition – that often see
people eventually losing their jobs, becoming withdrawn and not engaging in
everyday activities – are known as hypomanic states.
Bipolar disorder – a mood disorder characterised by polar
extremes of mood – was once known as “manic-depressive disorder”, which sheds light on the symptoms of this often debilating psychiatric condition.While it is normal to experience fluctuating periods of happiness and sadness associated with usual life circumstances, a
person diagnosed with bipolar disorder will have triggered swings from extreme
happiness and high levels of energy, to extreme sadness and hopelessness,
within a matter of hours or days. Extreme happiness presents as mania, such
that a person becomes excessively active in behaviour and speech, finds it
difficult to sleep or sit still without fidgeting, and may have racing thoughts
and ideas that fly quickly through the mind in illogical succession. A person in the manic phase may take more
risks, such as being more sexually active, taking drugs or spending more
money. Compare the manic phase to
extreme sadness, where a person may experience debilitating depression and
limited energy. During the depressive
phase a person may sleep all day and feel as if everything in their world is
hopeless, with no motivation to change things. Both extremes are like a see-saw
for the individual with bipolar disorder, who will likely experience no sense
of organisation or control over their life. The extremes of bipolar disorder
are associated with fluctuating neurotransmitter levels in the brain – a
significant rise in dopamine levels for mania and a significant drop in
serotonin and opioid levels for depression.
Less extreme versions of this debilitating condition – that often see
people eventually losing their jobs, becoming withdrawn and not engaging in
everyday activities – are known as hypomanic states.
It is important to remember that victims of domestic and
emotional abuse may appear – or are led to believe that they are – behaving in
a manner akin to bipolar disorder, and if this is happening to you it is vital
to seek urgent support. A correct diagnosis of bipolar disorder does not stem
from a disgruntled partner, an ex or a psychopathic boss, who may gain pleasure
in causing upset and confusion – a manipulative tactic known in modern parlance
as gaslighting – but rather stems from meeting strict criteria in the
Diagnostic and Statistical Manual Version 5 (DSM-5). The DSM-5 can be relied
upon – as the bible of psychiatrists – to determine real cases of psychiatric
disorder, so that the individual sufferer can receive vital treatment (such as
pharmacotherapy or counselling) to improve their quality of life. The DSM-5 recognises four main types of
bipolar disorder. The first is Bipolar I
Disorder, where manic episodes last for at least 7 days and severely consume
the energy resources of the individual, to the point where they may need
hospitalisation. Depressive symptoms usually co-occur for around 2 weeks and
may also be present during episodes of mania.
The second is Bipolar II Disorder, which is defined as a successive
pattern of unprovoked depressive symptoms and hypomanic states that cycle for
at least 7 days, and might even surprisingly occur at the same time. The third is Cyclothymic Disorder (also
called cyclothymia), defined by numerous periods of hypomanic and depressive
episodes lasting consecutively for at least 2 years (1 year in children and
adolescents). Finally, Unspecified Bipolar Disorder is a catch-all category,
where a person may exhibit episodes of mania or depression, but not usually
within the same timescales as the main diagnoses.
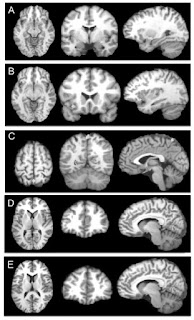
What then, are the neuroscientific bases of a DSM-5
diagnosis of bipolar disorder – in other words, which brain regions are more
activated in the MRI scanner? Recent studies of bipolar disorder have
demonstrated, particularly in response to emotional stimuli like faces, that an
over-active connectivity occurs between the amygdalae and prefrontal cortex –
brain regions associated with arousal/fear and goal-directed behaviours
respectively. This suggests that people with bipolar disorder may not be able
to effectively self-regulate their emotional responses to their
environment. Such hyperactivity in the
brain may also be associated with learned responses that began during
significant past trauma, or may even be due to the increasingly stressful, busy
and socially-isolated lives we lead today.
For example, chronic trauma, stress and social isolation (e.g. due to
long working hours and parental separation) may cause a downregulation
(reduction) of opioid receptors in the brain – the locks to the pain-relieving
brain hormone keys. Opioids are the brain’s natural defense to pain – including
emotional pain – and so if chronic emotional pain is experienced, opioids may
become less potent over time. We also
release opioids and other hormones, such as oxytocin, during intimate
pair-bonding. If emotional and/or
physical abuse is chronically experienced, a person may begin to exhibit more
and more signs akin to emotional dysregulation and bipolar disorder.
 And so, if you are a friend or family of a person who may be
exhibiting manic or depressive coupled with periods of low
energy and hopelessness, in a cyclical pattern over long periods, with no
obvious cause, it might be useful to do the following. First, gently communicate with the person, to
try to establish if there are serious, underlying causes for this behaviour,
such as physical or emotional abuse (don’t simply assume that they are suffering
from bipolar disorder). Be prepared that
the person may not wish to open up immediately, but be supportive and
accepting. If no obvious cause for the
behaviour is established, then the second step might be to suggest the person
visit a psychotherapist, to talk through with a trained professional who can
establish the cause. Finally, with the
help of the therapist, a formal diagnosis for the behaviour can be established
and treated, usually with a combination of suitable medication and further
psychotherapy.
And so, if you are a friend or family of a person who may be
exhibiting manic or depressive coupled with periods of low
energy and hopelessness, in a cyclical pattern over long periods, with no
obvious cause, it might be useful to do the following. First, gently communicate with the person, to
try to establish if there are serious, underlying causes for this behaviour,
such as physical or emotional abuse (don’t simply assume that they are suffering
from bipolar disorder). Be prepared that
the person may not wish to open up immediately, but be supportive and
accepting. If no obvious cause for the
behaviour is established, then the second step might be to suggest the person
visit a psychotherapist, to talk through with a trained professional who can
establish the cause. Finally, with the
help of the therapist, a formal diagnosis for the behaviour can be established
and treated, usually with a combination of suitable medication and further
psychotherapy.
The ultimate take-home message is this: don’t be quick to
give a layman’s diagnosis to a person who may exhibit symptoms akin to bipolar
disorder, as there may be other reasons for their behaviour. However, if a formal diagnosis by a trained professional
is established, a person suffering with bipolar disorder has a wealth of
treatment options available to him or her, that can enable them to continue
living a fullfilling, enjoyable life! We
must always remember: life is too short and too precious to cause - or
exacerbate - human suffering!
Dr Samantha Brooks is a neuroscientist at the UCT Department
of Psychiatry and Mental Health, specialising in the neural correlates of
impulse control from eating disorders to addiction. For more information on neuroscience at UCT
and to contact Samantha, see www.drsamanthabrooks.com. Note: Images royalty
free, courtesy of https://commons.wikimedia.org/wiki.